
Does the vaccine rollout mean it’s back to normality for the healthcare community?
The healthcare landscape has been under considerable strain over the past 18 months. This time last year, we were just beginning to process the potential long-term impact caused by COVID-19 on healthcare providers, but what this means for the medium to long term is still uncertain.
As some industries across the globe are gradually starting to regain a glimmer of normality, health care professionals (HCPs) are still under significant pressure to cope with the backlog of missed clinic time with their patients, deal with uncertainty and continue to adjust to the ‘new normal’.
So, what are the key challenges that HCPs are continuing to face?
What does this mean for pharma?
1/ Burden on resource is high, and it isn’t going away any time soon
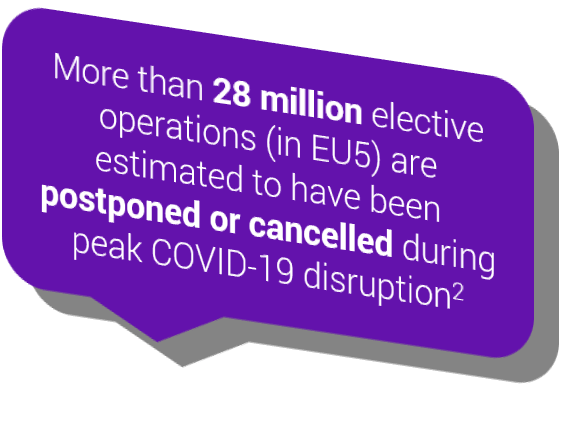
The reduction in access to patients (around a third less consultations in 2020 vs 2019)1 has understandably led to a significant backlog of cases, which some analysts estimate will take up to a year to make up. In addition, missed diagnoses, delays in treatment initiation and a potential long-term increase in new ‘advanced or complex’ cases all imply that the burden on resource isn’t going away any time soon.
While pharma looks to reignite their customer relations, physicians may be looking to claw back lost time.
Now more than ever, pharma needs to make every interaction count – a perfect opportunity to refocus their engagements on what really matters most.
So, what does matter most?
We can’t assume that what’s most important today is the same as 18 months ago, or indeed what will be most important in 18 months’ time.
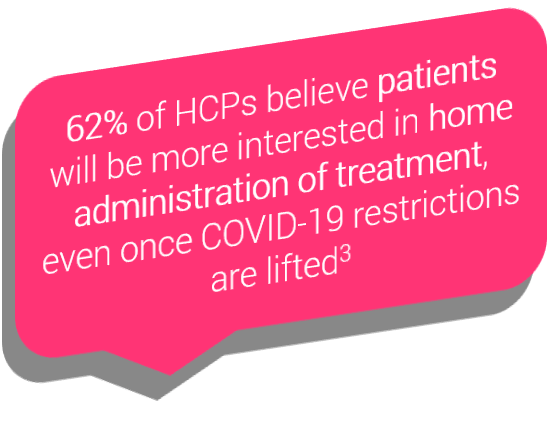
For example, we’ve observed shifts in prescribing across multiple therapy areas, in favour of options that allow home administration, less hands-on monitoring and fewer hospital visits. Whilst this provides an unexpected opportunity for pharma brands that are able to elevate these benefits, those with complex regimens or burdensome monitoring may require a new strategy.
It is key for pharma medical and brand teams to understand the root cause of changing behaviour and develop strategies to reassure and support their customers and patients moving forward.
2/ While telemedicine has supported a change in patient management, the immediate benefits don’t always translate into patient outcomes
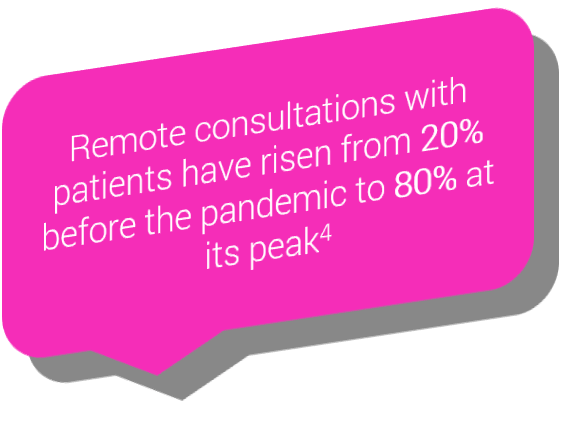
One of the greatest areas of adaption has been the sudden rise in virtual consultations. At its peak, these made up to around 80% of all outpatient appointments.
Although we’re now seeing a return to in-person consults, the expectation is that telemedicine will be here to stay.
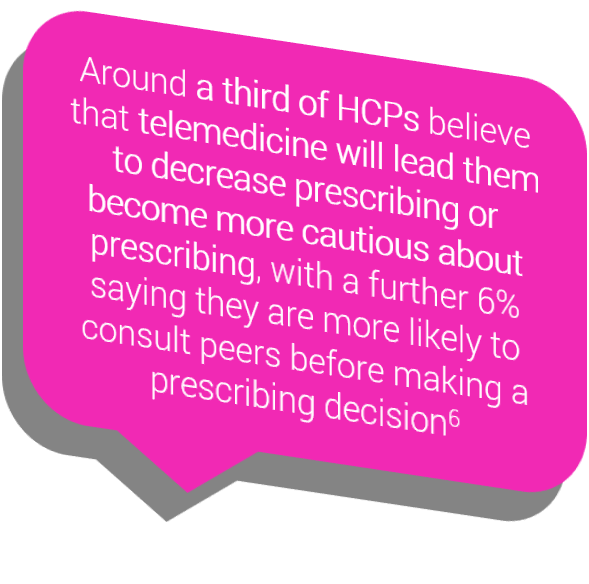
While there are numerous benefits associated with telemedicine, its adoption also has a number of disadvantages, particularly in supporting diagnoses, physical examinations, and remaining connected with patients with limited access/knowledge of digital solutions.
For example, NHS digital figures show that before the pandemic, in 2019, nearly 40%5 of individuals had no access to online consultations, limiting their access to adequate healthcare in an advancing telemedical society. Even patients with access may be unfamiliar or uncomfortable using it, potentially impacting opportunities to be diagnosed by HCPs. While the pandemic has seen a shift in adoption, there are still patients where these drawbacks can and will lead to health inequities, as these advances often favour the younger, technical-savvy, more affluent members of society.
Another drawback is that HCPs themselves may not be convinced or confident enough to translate their face-to-face clinical practice into meaningful virtual exchanges. One study of surveyed HCPs showed that about a fifth reported being reluctant to initiate new or change current treatment without having a face-to-face consultation with a patient.2
Alongside the advances in remote communications, the evolution of artificial intelligence (AI) within telemedicine approaches means that this too will increasingly become part of the ‘new normal’. The ability of the healthcare community to adequately react, evaluate and respond to such tools will rely on HCPs becoming as comfortable with AI algorithms as they are with physical examinations.
It is important for pharma to support HCPs in this transition and to navigate this new dynamic, while identifying the barriers to virtual diagnosis and prescribing.
3/ While the pressure to meet the demand for online delivery of medical information was already high pre-COVID-19, the urgency to deliver digital engagement models that change behaviours is now accelerating exponentially
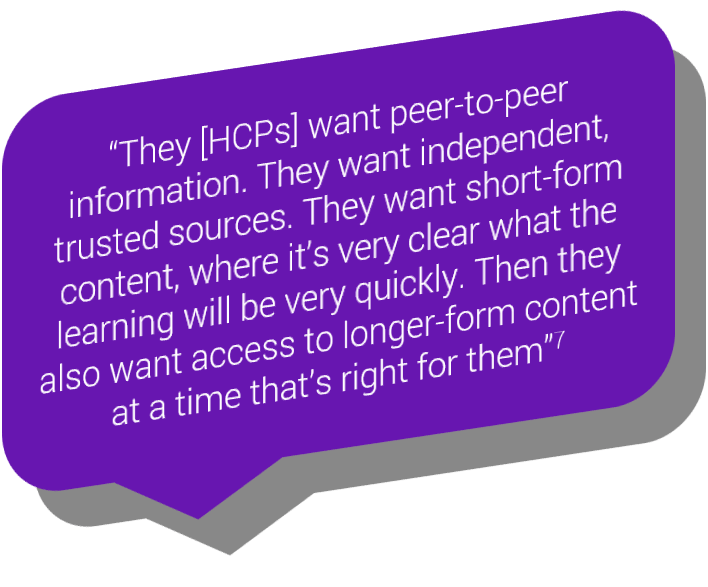
Successful digital engagement requires careful thought. Communications should be designed specifically to target and help shape behaviour, with user journeys personalised and reflective of their needs.
For example, content that was once intended for an in-person HCP adboard will require a change in engagement strategy to deliver the same kind of impact online. A physician interview video that is buried in a website and 20 minutes long is unlikely to be found or watched.
The increased focus (enhanced by the impact of the COVID-19 pandemic) on the personalisation and practicalities of healthcare delivery also means there is an increasing need to differentiate medical information based on outcomes. HCPs also want to have immediate access to this content, as well as the ability to retain and reuse it for the future.
The real challenge for pharma is to address the question of whether, or more precisely how, digital strategies can provide HCPs with the same level of content, engagement, and influence as peer-to-peer events.
The internet is becoming a more utilised channel, with restrictions in face-to-face interactions for HCPs meaning their behaviours are already being influenced by what they find online, whether from pharmaceutical companies or other providers occupying the same space.
But it needs to be relevant.
In a recent survey, 58% of HCPs agreed that at least one pharma company has ‘spammed’ them with digital content during the COVID-19 pandemic.3
Through AI-lead learning, it is now possible to engage, educate and positively impact HCPs online, in ways that deliver a more personal touch. These methods of user centricity have already been successfully adopted in other industries at a much faster rate than pharma. Companies like Amazon are leading the way in influencing behaviour through personalised customer journeys.
It is important for pharma to recognise the digital information consumption needs of HCPs and build targeted engagement strategies that supplement practical support for their patients, and build relationships with digital health innovators to produce new innovative digital solutions.
Key takeaways
Understanding changing mindsets and behaviours
Adapting and supporting the shift in the direction of telemedicine
Exploring and investing in the power of digital strategies
References
- Syneos Heath Communications 2021: Telemedicine Use and Field Force Engagement in the COVID-19 Era and Beyond, viewed June 2021
- IQVIA 2021: Monitoring the Impact of COVID 19 on the Pharmaceutical Market EU4 & UK, viewed June 2021
- Accenture May 2020: Reinventing Relevance: New Models for Pharma Engagement with Healthcare Providers in a COVID-19 World. Accenture Healthcare Provider Survey May 2020, viewed June 2021
- Sermo 2020: HCP Sentiment Study Series - part 1, viewed June 2021
- Mustafa H et al. 2020, A Commentary on “Impact of the Coronavirus (COVID-19) pandemic on surgical practice – Part 1”, International Journal of Surgery, vol. 83, pp. 115–116.
- Syneos Health 2020: COVID-19 Pandemic Fuels Surge in Telemedicine and Virtual Field Force Engagements, viewed June 2021
- EPG Health 2020: Cutting Through the Noise for HCPs, viewed June 2021





